Vulvar Dermatological Conditions
Just one Google search with the keyword “vagina” and a countless number of words automatically follow to complete the sentence. Some of these include “vagina itch”, “vagina discharge”, “vagina burning”, and even “vagina cancer”. I shudder to think how many people are searching online for generic guidance on their vaginal symptoms or possible vulvar dermatological conditions. The accessibility of vaginal creams, douches, and yeast treatments at the local pharmacy, paves the way for improper diagnosis or even the potential for covering up symptoms that need to be assessed and treated by a knowledgeable physician or gynaecologist.
I spend a considerable amount of time with my clients encouraging them to normalize looking and investigating their own genital anatomy on a regular basis. This should be a common practice indoctrinated in our children. Just like we need to do regular breast, testicular, and mole checks for changes, the same rules apply for our genitals. This assures us the gift of early detection of colour changes, structural changes and potential abnormal growths. These changes may be totally benign, but I encourage you to allow your physician, with many more years of experience and who doesn’t rely on a Google image, to determine this.
It is helpful to begin by learning more about a few common dermatological conditions that can develop in and around the genital area.
Lichen Sclerosus
Lichen Sclerosus (LS) is a persistent, inflammatory mucocutaneous disorder of the genital area. It commonly involves the inner areas of the vulva (non hair bearing area). It can be localized to one area or spread throughout the perineum, labia minora, and clitoral hood. LS is commonly associated with a “figure of 8” pattern distribution of white, dry, thick plaques of “crinkly” skin around the anogenital area but typically does not extend into the vagina. Over time, LS may result in labia minora resorption, phimosis of the clitoral hood, scarring and fissuring of the skin around and near the vaginal opening. Symptoms include severe itch, burning, dysuria, and dyspareunia in women and men, although LS is 10x more prevalent in the female population. It is imperative to be regularly monitored by a specialist as those with LS have a slightly increased risk of developing squamous cell carcinoma. Early diagnosis and detection of LS helps ensure that appropriate medications are used to prevent the worsening of LS symptoms.
https://www.obstetrics-gynaecology-journal.com/article/S0957-5847(05)00002-8/fulltext
Lichen Planus (LP)
Lichen Planus (LP) is an autoimmune, inflammatory disease that typically affects the skin, nails, and hair. It can also involve the mucosal surfaces of the mouth, nose and esophagus. The genital component is often missed or misdiagnosed. Unlike LS, LP often involves the vaginal mucosa which is located at the introitus and inside the vaginal canal. It affects the squamous epithelium of the vulva and causes ulcerations in the vestibule (Wickham’s stria). LP also affects the mucous membrane of the mouth. This presents as a painless, lacy network of white streaks and/or painful ulcers on the inside of the cheek, gums, or tongue. Genital symptoms include increased vaginal discharge, burning, itch, and dyspareunia. Over time, resorption of the labial architecture may occur. The cause of LP is not known but may be due to an allergic or immune reaction. Risks for the development of LP include hepatitis C and exposure to certain medicines, dyes, and other chemicals (including gold, antibiotics, arsenic, iodides, chloroquine, quinacrine, quinine, phenothiazines, and diuretics). LP is most common in middle-aged adults and less common in children.
https://www.researchgate.net/publication/323480912_Vulval_lichen_planus-lichen_sclerosus_overlap
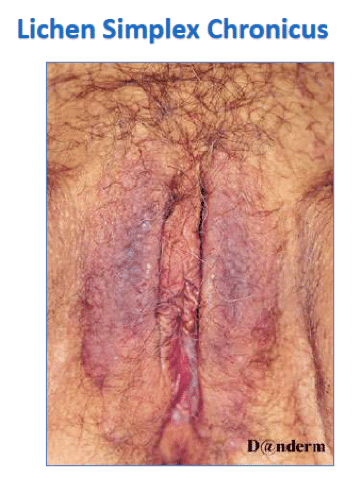
Lichen Simplex Chronicus (LSC)
Lichen Simplex Chronicus (LSC) is a genital skin condition caused by long term persistent itching and scratching of the tissues around the vulva and vagina. The initial itch may be a result of microtrauma to the skin from friction or rubbing or a sensitivity to a perfume or chemical in clothing that is in close contact with the genital area. Over time, an “itch-scratch” cycle is established, often during sleep, in which the scratching causes the skin to thicken and look leathery in texture, which leads to more itching. LSC may occur in those who have skin allergies, eczema, or psoriasis. This condition may occur in adults as well as children. Treatment focuses on behavioural strategies and vulvar hygiene to eliminate further irritants coming in contact with the genital area. Medications like steroid ointments or oral medications are often prescribed to help resolve the inflammation.
Genitourinary Syndrome of Menopause
Genitourinary syndrome of menopause (GSM) is associated with changes in vulvar and lower urinary tract anatomy due to menopause-related decreases in estrogen and other hormones. It is believed within 3 years of the onset of menopause, 50% of individuals will experience GSM symptoms. Symptoms include vaginal or vulvar dryness, burning, itching, dyspareunia, bleeding, vaginal discharge, urinary urgency, urinary frequency, and recurrent urinary tract infections. GSM symptoms can also occur during a hypoestrogenic time in life including those who are early postpartum and breastfeeding as well as those taking anti estrogen medications for cancer treatments. The vulva and vaginal opening typically presents as thin, pale in colour, decreased lubrication, and erythematous. The vaginal opening may be narrowed with evidence of labia minora resorption. Treatment may include vulvar and vaginal moisturizers and/or low dose intravaginal hormone therapy. Pelvic physiotherapy plays a relevant role in this condition through guidance on pelvic floor muscle training and education on optimizing bladder, bowel, and sexual function.
https://link.springer.com/chapter/10.1007/978-3-319-42677-8_8
Pelvic floor physical therapy plays a valuable role in supporting the management of many dermatological conditions through vulvar hygiene education to reduce potential skin irritants that may aggravate symptoms. Goals include optimizing the mobility and elasticity of the vulvovaginal tissues, promoting blood flow to the tissues, optimizing strength of the pelvic floor muscles, and education around ideal toileting habits and strategies to avoid straining.
The vulvovaginal dermatological conditions described above are common but this is certainly not an exhaustive list of all of the conditions that involve the genital area. What is important here is to recognize how a vast array of vulvovaginal disorders include similar symptoms. In conclusion, all things that “itch” are not necessarily a yeast infection and warrant a thorough check up by a trained physician or specialist to ensure appropriate and timely management of the condition.
References:
https://www.cancertherapyadvisor.com/home/decision-support-in-medicine/obstetrics-and-gynecology/vulvovaginal-disorders-lichen-planus/
https://www.slucare.edu/ob-gyn/female-pelvic-medicine-and-reconstructive-surgery/vulvar-and-vaginal-disorders-specialty-center.php
https://www.aafp.org/dam/AAFP/documents/journals/afp/Ringel.pdf
https://dermnetnz.org/topics/lichen-sclerosus/